Narcolepsy: Causes, Treatments, and What You Need to Know
When you think of narcolepsy, a chronic neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. Also known as sleep disorder with cataplexy, it doesn’t just make you sleepy—it can knock you out mid-sentence, mid-step, or even while laughing. This isn’t normal tiredness. People with narcolepsy experience sudden, uncontrollable sleep attacks during the day, even after a full night’s rest. It’s not laziness. It’s not poor sleep habits. It’s a real, measurable brain condition tied to low levels of hypocretin, a chemical that helps keep you alert.
Narcolepsy often shows up with other symptoms like cataplexy, a sudden loss of muscle control triggered by strong emotions like laughter or anger. You might drop your coffee cup, slump in your chair, or even collapse—without losing consciousness. Then there’s excessive daytime sleepiness, the constant, overwhelming urge to nap, no matter how much you’ve slept. Some people also see hallucinations when falling asleep or waking up, or feel paralyzed for a few seconds after waking. These aren’t scary stories—they’re common signs doctors look for.
Most people with narcolepsy are diagnosed in their teens or 20s, but many go years without answers. Doctors use sleep studies, blood tests, and symptom tracking to confirm it. Treatment isn’t one-size-fits-all. Some rely on modafinil, a wakefulness-promoting drug that helps reduce daytime sleepiness without the jitteriness of stimulants. Others use sodium oxybate, antidepressants for cataplexy, or lifestyle tweaks like scheduled naps and strict sleep routines. There’s no cure yet, but with the right plan, most people can manage symptoms and live full lives.
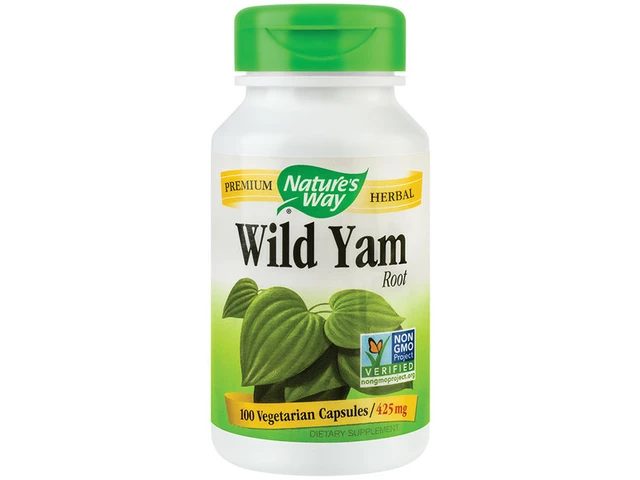
The posts below cover real-world connections you might not expect. You’ll find how narcolepsy overlaps with depression, why some sleep meds affect heart health, and how medications used for blood pressure or diabetes can sometimes help—or hurt—sleep regulation. You’ll also see how supplements like L-tryptophan, often used for mood, can interact dangerously with sleep disorder treatments. This isn’t just about sleep. It’s about how your brain, your meds, and your daily choices all tie together. What you find here isn’t theory—it’s what people actually deal with, and how they’ve learned to cope.