Every year, over 100 million Americans deal with acute diarrhea. While it's often short-lived, knowing when to reach for OTC remedies versus when to call a doctor matters. OTC diarrhea treatments like loperamide and bismuth subsalicylate can help, but misuse can lead to serious issues. This guide explains exactly when to use them and when to seek professional help.
The Two Main OTC Options
Loperamide is a synthetic opioid agonist that works by slowing intestinal movement. It's available under brand names like Imodium. The standard adult dose is 4mg after the first loose stool, followed by 2mg after each additional loose stool, not exceeding 8mg in 24 hours. Loperamide reduces stool frequency by 40-60% within 24 hours when used properly.
Bismuth Subsalicylate (sold as Pepto-Bismol or Kaopectate) works through four mechanisms: coating the gut lining, absorbing toxins, reducing inflammation, and fighting bacteria. Each 30mL liquid dose contains 262mg of bismuth. It's particularly effective for diarrhea with nausea or stomach cramps.
Age restrictions matter here. Imodium's liquid form is FDA-approved for children 6+, while caplets are for 12+. Pepto-Bismol's Children's formula is for ages 12+. Never give adult-strength versions to younger kids without a doctor's approval.
When to Use OTC Treatments
OTC medications work best for mild, short-term diarrhea. Use them when:
- You have fewer than four loose stools per day
- No fever above 100.4°F (38°C)
- No blood or black stools
- Diarrhea has lasted less than 48 hours
- You're not experiencing severe dehydration symptoms (dizziness, very dark urine)
For example, if you get traveler's diarrhea from a new food but feel otherwise fine, taking loperamide or bismuth subsalicylate can help you feel better quickly. A 2022 Journal of Travel Medicine study found bismuth subsalicylate reduces traveler's diarrhea risk by 65% when taken prophylactically.

When to See a Doctor
Stop using OTC meds immediately and call a doctor if you experience any of these red flags:
- Fever higher than 101.3°F (38.5°C)
- Bloody or black stools (indicating possible internal bleeding)
- Severe abdominal pain or swelling
- Diarrhea lasting more than 48 hours
- Signs of dehydration: dry mouth, little to no urine output, or extreme fatigue
The Mayo Clinic's 2023 guidelines state: 'Do not use anti-diarrheals for diarrhea lasting more than 48 hours, accompanied by fever, bloody stools, or severe abdominal pain.' The CDC reports 15-20% of infectious diarrhea cases involve fever or bloody stools, which require medical evaluation to rule out serious infections like C. diff or inflammatory bowel disease.

Common Mistakes and Risks
Many people misuse OTC diarrhea meds. Here are the biggest dangers:
- Overdosing loperamide: Taking more than 8mg in 24 hours can cause dangerous heart rhythm problems. The FDA warned in 2016 about loperamide abuse linked to 48 cardiac deaths between 1976-2015.
- Combining medications: Using both loperamide and bismuth subsalicylate together increases salicylate toxicity risk. One Drugs.com reviewer reported 'took 6 caplets in 4 hours - ended up in ER with severe constipation' (verified October 12, 2023).
- Using for viral or bacterial infections: Loperamide can trap pathogens in your gut, worsening infections. Dr. Kyle Staller, a Massachusetts General Hospital gastroenterologist, emphasizes: 'Take [anti-diarrheals] as directed, but avoid them if you have a fever or bloody diarrhea, as they can prolong infection by trapping pathogens.'
| Medication | How It Works | Best For | Key Risks |
|---|---|---|---|
| Loperamide | Slows intestinal movement by binding to opioid receptors | Quick relief for watery diarrhea | Constipation, cardiac issues at high doses |
| Bismuth Subsalicylate | Covers gut lining, absorbs toxins, fights bacteria | Diarrhea with nausea or cramps | Blackened stools/tongue, salicylate toxicity |
Home Care Tips
OTC meds alone aren't enough. Pair them with these evidence-based home care steps:
- Hydrate properly: Use oral rehydration solutions (75mmol/L sodium) per WHO guidelines. Avoid sugary drinks like soda or juice-they worsen diarrhea.
- Try the BRAT diet: Bananas, rice, applesauce, and toast are gentle on the gut. A 2022 American Academy of Pediatrics survey found 92% of pediatricians recommend this for kids.
- Avoid dairy and high-fiber foods: These can irritate the digestive system during acute episodes.
- Rest: Your body needs energy to fight whatever caused the diarrhea.
Remember: OTC treatments manage symptoms but don't cure the underlying cause. If symptoms persist after 48 hours, see a doctor to identify the real issue.
Can I take loperamide and Pepto-Bismol together?
No, combining loperamide and bismuth subsalicylate (Pepto-Bismol) is not recommended. Bismuth subsalicylate contains salicylates, which can increase the risk of side effects when taken with other medications. Additionally, taking multiple anti-diarrheals can lead to overdosing and complications like constipation or toxicity. Always follow the dosage instructions on the label and consult a healthcare provider if unsure.
Why does Pepto-Bismol turn my stool black?
Bismuth subsalicylate reacts with sulfur compounds in your digestive tract, causing harmless temporary black stools and tongue discoloration. This occurs in 98% of users according to Pepto-Bismol's prescribing information. It's not dangerous, but if you're unsure, check with a doctor to rule out actual bleeding.
Is it safe to use OTC diarrhea meds for kids?
For children under 6, never use loperamide without a doctor's prescription. Pepto-Bismol's Children's formula is safe for ages 12+, but younger kids need pediatrician approval. The NHS warns against loperamide for children under 12 due to risk of paralytic ileus, citing 127 pediatric adverse event reports to the FDA between 2010-2020.
What should I do if OTC meds don't work?
Stop using OTC treatments immediately and see a doctor. Persistent diarrhea could indicate serious conditions like infections (C. diff, salmonella), inflammatory bowel disease, or food intolerances. The American Gastroenterological Association's 2023 update recommends medical evaluation for diarrhea lasting more than 48 hours, especially with dehydration signs.
Can I use OTC meds for chronic diarrhea?
No. Chronic diarrhea (lasting over 4 weeks) requires medical diagnosis and treatment. OTC anti-diarrheals mask symptoms but don't address underlying causes like irritable bowel syndrome, celiac disease, or pancreatic issues. The FDA specifically warns against using loperamide for chronic conditions without medical supervision.

 Top Alternatives to Metformin: Exploring Options for Diabetes Management
Top Alternatives to Metformin: Exploring Options for Diabetes Management
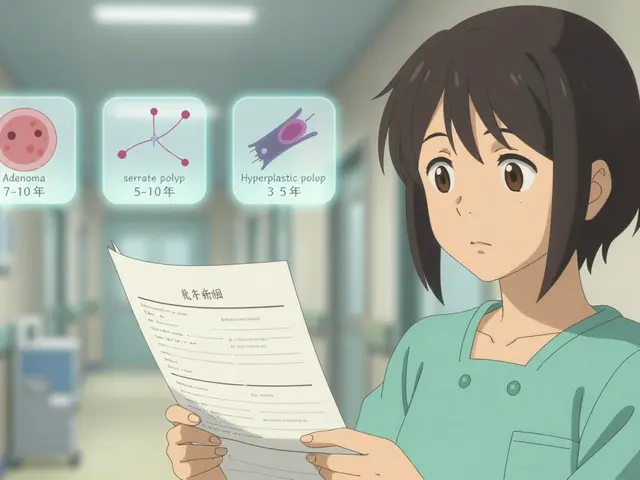 Repeat Colonoscopy: What Your Surveillance Interval Should Be After Polyp Removal
Repeat Colonoscopy: What Your Surveillance Interval Should Be After Polyp Removal
 What to Do If a Child Swallows the Wrong Medication: Immediate Steps That Save Lives
What to Do If a Child Swallows the Wrong Medication: Immediate Steps That Save Lives
 OTC Diarrhea Treatments: When to Use and When to See a Doctor | Safe Self-Management Guide
OTC Diarrhea Treatments: When to Use and When to See a Doctor | Safe Self-Management Guide
 The History of Bisoprolol Fumarate: From Discovery to Medical Use
The History of Bisoprolol Fumarate: From Discovery to Medical Use
Sarah B
February 6, 2026 AT 21:45OTC meds are dangerous period
Tola Adedipe
February 7, 2026 AT 13:47Loperamide is risky. People take too much. Always check dosage.
Eric Knobelspiesse
February 8, 2026 AT 08:09Loperamide is dangereous but sometimes nessesary. Like fire, it's a tool. But misuse burns you. Just sayin'.
Heather Burrows
February 9, 2026 AT 10:37Some people just don't read the instructions. It's not hard. But they do it anyway. Classic.
Ritu Singh
February 11, 2026 AT 00:30It's important to use OTC meds correctly. But also know when to seek help. Balance is key.
Mark Harris
February 11, 2026 AT 22:22Stay hydrated! Drink water and electrolytes. Don't panic. You got this!
Savannah Edwards
February 13, 2026 AT 09:28When dealing with diarrhea, staying hydrated is super important.
But it's not just about chugging water.
The WHO recommends oral rehydration solutions with 75mmol/L sodium.
Sugary drinks like soda or juice can actually make things worse by drawing more water into the intestines.
The BRAT diet-bananas, rice, applesauce, toast-is gentle on the stomach.
But it's not a cure-all; it's just for symptom management.
Avoid dairy and high-fiber foods during an episode.
Rest is essential because your body is fighting something.
If you have bloody stools or a high fever, you need to see a doctor immediately.
OTC meds like loperamide can help, but only if used properly.
Taking too much can cause serious heart issues.
Bismuth subsalicylate is good for nausea and cramps but can turn your stool black.
It's harmless but might scare you.
Remember, OTC meds don't treat the cause, just the symptoms.
If it lasts more than 48 hours, get checked out.
Stay safe out there.
Mayank Dobhal
February 13, 2026 AT 18:02Diarrhea is gross. No meds needed. Just tough it out.
Marcus Jackson
February 15, 2026 AT 01:05You need to know the difference between acute and chronic. OTC meds are for short-term only. Chronic needs medical attention.
Natasha Bhala
February 15, 2026 AT 11:49You're right about hydration. Drink plently of water and maybe some electrolyte drinks. And remeber to rest. You'll feel better soon. Stay positive!
Gouris Patnaik
February 16, 2026 AT 08:28US people always overuse meds. In my country, we just use home remedies. No need for fancy pills.