Quick Takeaways
- Cefaclor is a second‑generation cephalosporin that can be useful for selected ICU infections when resistance patterns allow.
- Standard adult dosing is 250‑500 mg every 8 hours, but severe renal impairment requires a 50‑75 % dose reduction.
- Watch for cross‑reactivity with penicillins and avoid use in patients with known cephalosporin allergy.
- Integrate cefaclor into stewardship protocols only after confirming susceptibility; it’s not a first‑line drug for sepsis.
- Always double‑check drug‑interaction alerts, especially with oral anticoagulants and certain diuretics.
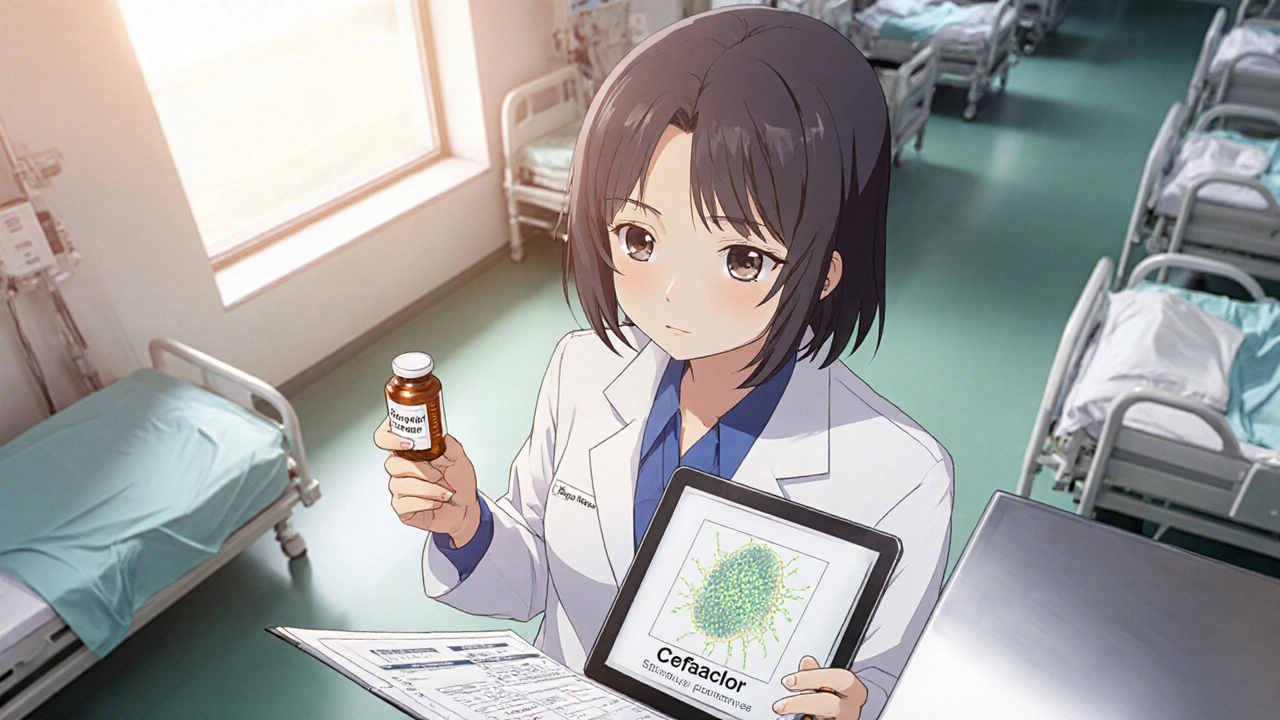
What is Cefaclor?
When you hear the name Cefaclor is a second‑generation β‑lactam cephalosporin that was first approved by the FDA in 1979. It works by disrupting bacterial cell‑wall synthesis, which makes it bactericidal against a range of gram‑positive and some gram‑negative organisms. Because it’s taken orally, you’ll often see it used for outpatient respiratory or skin infections, but its pharmacokinetic profile also lets it play a role in the hospital setting under the right circumstances.
Why Consider Cefaclor in the ICU?
ICU teams juggle a lot of antibiotics every day. So why pull cefaclor into that mix? A few reasons pop up:
- Targeted spectrum. When cultures show a susceptible organism like Streptococcus pneumoniae or Haemophilus influenzae, cefaclor can spare broader‑spectrum drugs and curb collateral damage.
- Oral step‑down. After the initial IV phase, you can switch to oral cefaclor without losing coverage, which shortens IV lines and frees up infusion pumps.
- Renal safety. Compared with many other cephalosporins, cefaclor’s renal clearance is predictable, making dose adjustments easier in patients with acute kidney injury (AKI).
That said, cefaclor isn’t a magic bullet. It doesn’t cover Pseudomonas, MRSA, or most Enterobacterales that often dominate ICU infections. So you’ll usually reserve it for documented, susceptible pathogens or as part of a de‑escalation strategy.
Dosing Strategies in Critical Care
Getting the dose right can be the difference between cure and resistance. Here’s a practical rundown:
- Standard adult dose: 250 mg‑500 mg every 8 hours (Q8H) for most infections.
- Severe infections: Some clinicians push to 500 mg Q8H for deep‑tissue infections, provided renal function is normal.
- Renal impairment: Adjust based on creatinine clearance (CrCl). See the table below for quick reference.
| CrCl (mL/min) | Recommended Dose | Frequency |
|---|---|---|
| ≥ 80 | 250-500 mg | Q8H |
| 50-79 | 250 mg | Q8H |
| 30-49 | 250 mg | Q12H |
| 10-29 | 125 mg | Q12H |
| <10 | Avoid use; consider alternative agent | - |
When you hit the <10 mL/min threshold, most guidelines advise against cefaclor because the drug may accumulate to toxic levels.
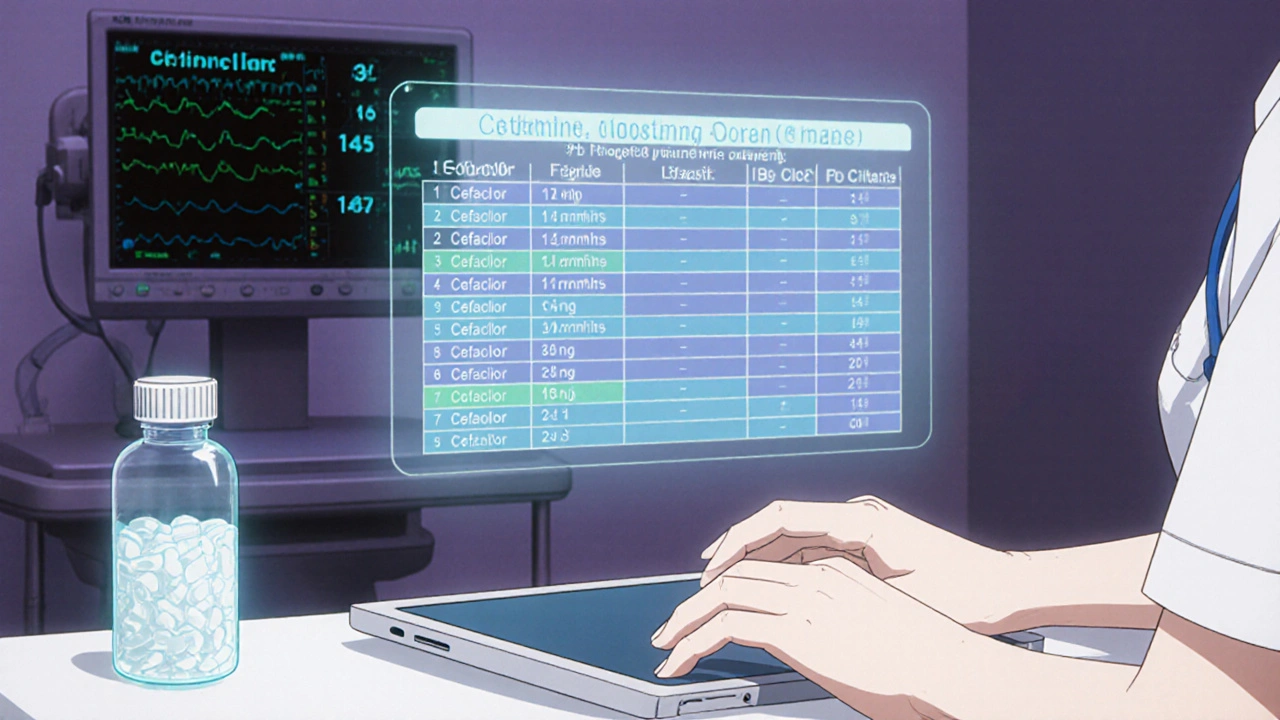
Renal Adjustment and Therapeutic Drug Monitoring
Even though cefaclor isn’t typically measured in serum, you can still watch for indirect signs of accumulation: sudden rise in bilirubin, unexplained nausea, or a new rash. In patients on intermittent renal replacement therapy, assume a 50 % dose reduction and monitor clinical response closely.
Drug Interactions and Safety Concerns
Because cefaclor is a β‑lactam, it can interfere with the gut flora that produces vitamin K. In rare cases, you might see an elevated INR in patients on warfarin. A quick check with the ICU pharmacist can catch this before it becomes a problem.
- Oral anticoagulants: Monitor INR when switching from IV penicillins to oral cefaclor.
- Probenecid: Can raise cefaclor plasma concentrations; avoid unless you purposefully want a higher exposure.
- Nephrotoxic agents: NSAIDs, aminoglycosides, and contrast media can worsen AKI, so adjust cefaclor dose sooner than you might otherwise.
Integrating Cefaclor into Antibiotic Stewardship
Stewardship programs thrive on narrowing therapy as fast as possible. Here’s how cefaclor fits:
- Start broad (e.g., piperacillin‑tazobactam) when sepsis is suspected.
- When cultures return S. pneumoniae with a MIC ≤ 2 µg/mL, de‑escalate to cefaclor.
- Document the switch, note the susceptibility, and set a stop date (usually 7‑10 days for uncomplicated pneumonia).
Because cefaclor’s oral formulation is cheap and well‑tolerated, it also helps reduce pharmacy costs and line‑associated complications.

Real‑World ICU Case Snapshot
Consider a 68‑year‑old male with COPD admitted for acute exacerbation. He’s intubated, develops a fever on day 2, and sputum cultures grow S. pneumoniae (penicillin‑susceptible, cefaclor MIC 1 µg/mL). Initial empiric therapy was meropenem. After 48 hours, the team steps down to cefaclor 500 mg Q8H because his CrCl is 65 mL/min. On day 5, his oxygenation improves, the chest X‑ray clears, and he’s switched to oral cefaclor 500 mg BID for the next five days before discharge.
This scenario illustrates three points: culture‑directed de‑escalation, easy oral step‑down, and cost savings without compromising outcomes.
Checklist for ICU Clinicians When Using Cefaclor
- Confirm pathogen susceptibility (MIC ≤ 2 µg/mL for most isolates).
- Assess renal function and apply the dosing table.
- Review the patient’s allergy history for β‑lactam cross‑reactivity.
- Check for interacting drugs (warfarin, probenecid, nephrotoxins).
- Document the de‑escalation rationale in the EMR.
- Plan oral step‑down when the patient is hemodynamically stable.
- Set a stop date and reassess daily for clinical response.
Frequently Asked Questions
Can cefaclor be used for Pseudomonas infections in the ICU?
No. Cefaclor’s spectrum does not cover Pseudomonas aeruginosa. For suspected or confirmed Pseudomonas, you’d need an anti‑pseudomonal agent such as cefepime, piperacillin‑tazobactam, or a carbapenem.
Is oral cefaclor as effective as IV therapy for severe pneumonia?
If the pathogen is susceptible and the patient has a functional GI tract, oral cefaclor achieves serum levels comparable to IV dosing for most respiratory pathogens. However, start with IV coverage until the patient is stable, then switch to oral as part of a step‑down strategy.
How do I adjust cefaclor for a patient on continuous renal replacement therapy (CRRT)?
CRRT clears cefaclor similarly to normal renal function, but the exact dose depends on filter type and flow rates. A practical approach is to use the 30‑49 mL/min CrCl bracket (250 mg Q12H) and monitor clinical response.
What adverse reactions should I watch for?
Common side effects include nausea, diarrhea, and rash. Rare but serious events are Stevens‑Johnson syndrome and drug‑induced liver injury. Any new rash or hepatic enzyme rise warrants immediate evaluation.
Is cefaclor safe in pregnant ICU patients?
Cefaclor is classified as Pregnancy Category B. Animal studies show no risk, and limited human data have not demonstrated fetal harm. Use only if the benefit outweighs any potential risk.
When you keep these points in mind, cefaclor can be a smart, cost‑effective piece of the ICU antibiotic puzzle. It isn’t a one‑size‑fits‑all drug, but with proper culture data, renal assessment, and stewardship oversight, it helps you hit the right balance between efficacy and safety.
 Buy Tamsulosin Online Safely: Where, How, and What You Need to Know
Buy Tamsulosin Online Safely: Where, How, and What You Need to Know
 Discover the Benefits of Coca: The Revolutionary Dietary Supplement
Discover the Benefits of Coca: The Revolutionary Dietary Supplement
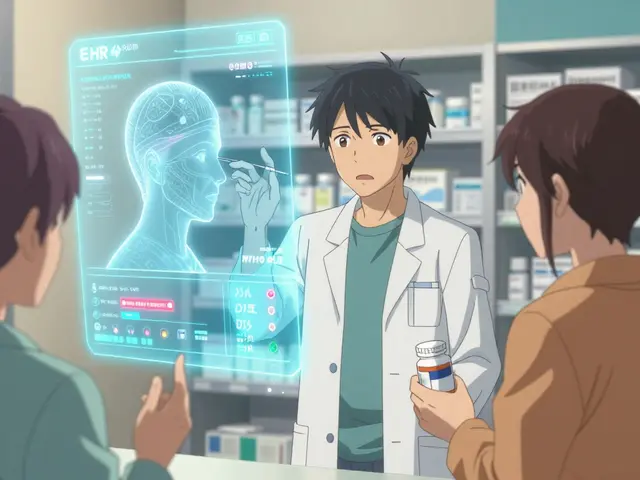 EHR Integration: How Pharmacy and Provider Systems Communicate for Safer Prescriptions
EHR Integration: How Pharmacy and Provider Systems Communicate for Safer Prescriptions
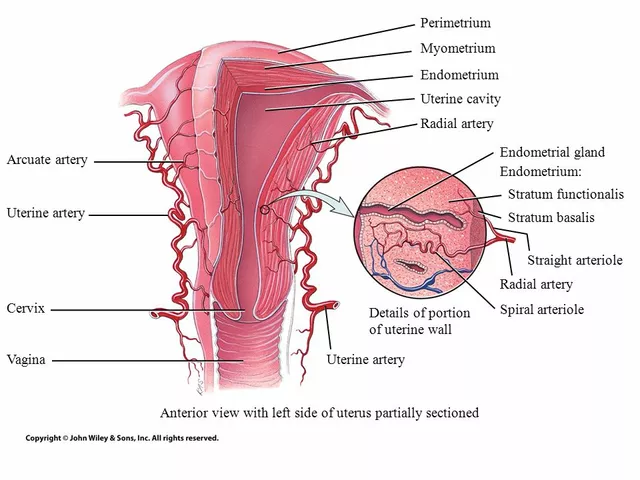 The Connection Between Overgrowth in the Uterine Lining and Migraines
The Connection Between Overgrowth in the Uterine Lining and Migraines
Olivia Harrison
October 24, 2025 AT 21:44Hey everyone, great rundown on cefaclor and its niche role in critical care. The fact that it’s oral makes it a handy step‑down option when cultures support a susceptible pathogen. I always start by verifying the patient’s renal function before committing to the standard 250‑500 mg q8h regimen. For CrCl above 80 mL/min the usual dose works fine, but once you dip below 50 mL/min you’ll want to pull back to 250 mg q8h. When the clearance falls into the 30‑49 mL/min range, extending the interval to q12h preserves efficacy while guarding against accumulation. In my ICU we’ve set a hard stop at CrCl < 10 mL/min because the exposure‑risk ratio becomes unfavorable. It also pays to double‑check for cross‑reactivity if the patient has a penicillin allergy; cefaclor shares the β‑lactam ring, though true IgE reactions are uncommon. Remember that cefaclor doesn’t cover Pseudomonas, MRSA, or most Enterobacterales, so it’s not a universal rescue drug. When the microbiology lab reports a susceptible Streptococcus pneumoniae, switching from IV ceftriaxone to oral cefaclor can free up a pump and reduce line‑associated complications. I’ve seen shorter ICU stays when we safely de‑escalate to oral agents early. Just keep an eye on drug‑interaction alerts, especially with warfarin, as cefaclor can modestly increase INR. The dose‑adjustment table you posted is spot‑on; I keep a laminated copy on my bedside computer for quick reference. For patients on diuretics, monitor electrolytes because shifts in volume can affect renal clearance. Finally, incorporate cefaclor only after susceptibility is confirmed and stewardship guidelines have approved its use. Stay safe and keep those cultures coming!
Bianca Larasati
November 3, 2025 AT 05:18Imagine the ICU as a battlefield where every antibiotic is a soldier-cefaclor can be the surprise ally that turns the tide when the enemy shows its true colors! Let’s champion its targeted spectrum and give broader drugs a well‑earned rest. Embrace the oral step‑down like a victory march, freeing up those precious IV lines. Together we can master de‑escalation and keep resistance at bay!
Corrine Johnson
November 12, 2025 AT 13:53Well… here we are again, wading through another “guide” that pretends to be groundbreaking-yet merely recycles textbook facts!!! The author omits the grim reality that cefaclor’s oral bioavailability can be erratic in critically ill patients; absorption may falter under vasopressor support… and yet, no mention of that? Moreover, the dosing table looks pristine, but who knows how it holds up when creatinine clearance is fluctuating hour by hour??? A true stewardship protocol would highlight these nuances, not mask them behind glossy bullet points.
Abhinav B.
November 21, 2025 AT 22:27Look, I get the point of using oral cefaclor but in real ICU you cant just switch after one dose-patients are often on pressors and gut perfusion is sketchy. If the gut ain't perfused, the drug won't get absorbed and you waste time. So watch the hemodynamics before you think of oral step‑down. Also, double check the allergy with penicilin cross reactivity-it's not a joke.
Abby W
December 1, 2025 AT 07:01Great summary! 👍 I love the clear dosing table 📊 and the reminder about renal adjustments. Using cefaclor as a step‑down can really cut down on line infections 🤒. Just remember to verify the culture results before switching! 😊
Zaria Williams
December 10, 2025 AT 15:35Yo, this is actually useful. The renal dosing chart is spot on. But real talk-most ICU docs still reach for broad‑spectrum IVs until the last minute. If you got a clean sputum culture you can definitely swing to cefaclor, saves time and lines.
ram kumar
December 20, 2025 AT 00:10Another generic antibiotic list, yawn.
Melanie Vargas
December 29, 2025 AT 08:44Hey team! 🌟 Remember, stewardship isn’t just about picking the right drug, it’s also about timing and patient factors. Cefaclor can be a solid choice when the bug is susceptible and the patient’s kidneys are cooperating. Let’s keep sharing culture data promptly so we can all de‑escalate safely! 🙌
krishna chegireddy
January 7, 2026 AT 17:18Everyone talks about cefaclor like it’s a safe bet, but the pharma push behind oral cephs is real. They want us to replace expensive IVs with cheap pills so they can boost profit margins. Use it only if you really know the bug, not because the protocol says so.
Max Lilleyman
January 17, 2026 AT 01:53Good that you listed the dosing, but the article glosses over the fact that cefaclor won’t cover many ICU bugs 😕. The step‑down is only safe after you have a documented susceptible organism 👩⚕️. Otherwise you’re just gambling.
Brett Witcher
January 26, 2026 AT 10:27The pharmacokinetic profile of cefaclor, notably its predictable renal clearance, justifies the straightforward dose‑adjustment scheme presented. However, the omission of pharmacodynamic targets such as %T>MIC limits the utility of the guide for optimizing exposure in severe infections.
Benjamin Sequeira benavente
February 4, 2026 AT 19:01Let’s cut to the chase-if the culture is clear, slam that oral cefaclor in and pull the IV lines now! No more hesitation, de‑escalate aggressively and protect those pumps. Your patients will thank you for the faster recovery.
Shannon Stoneburgh
February 14, 2026 AT 03:35This guide is too basic. It doesn’t tell you how to handle fluctuating creatinine or drug interactions beyond a vague warning. Need more depth.
Nathan Comstock
February 23, 2026 AT 12:10Honestly, anyone who thinks cefaclor is a miracle drug for the ICU is missing the bigger picture. The bacterial landscape in critical care is dominated by resistant gram‑negatives and requires agents with robust anti‑pseudomonal activity. Savvy clinicians reserve oral cephalosporins for truly narrow indications and never compromise on coverage when sepsis is in play.